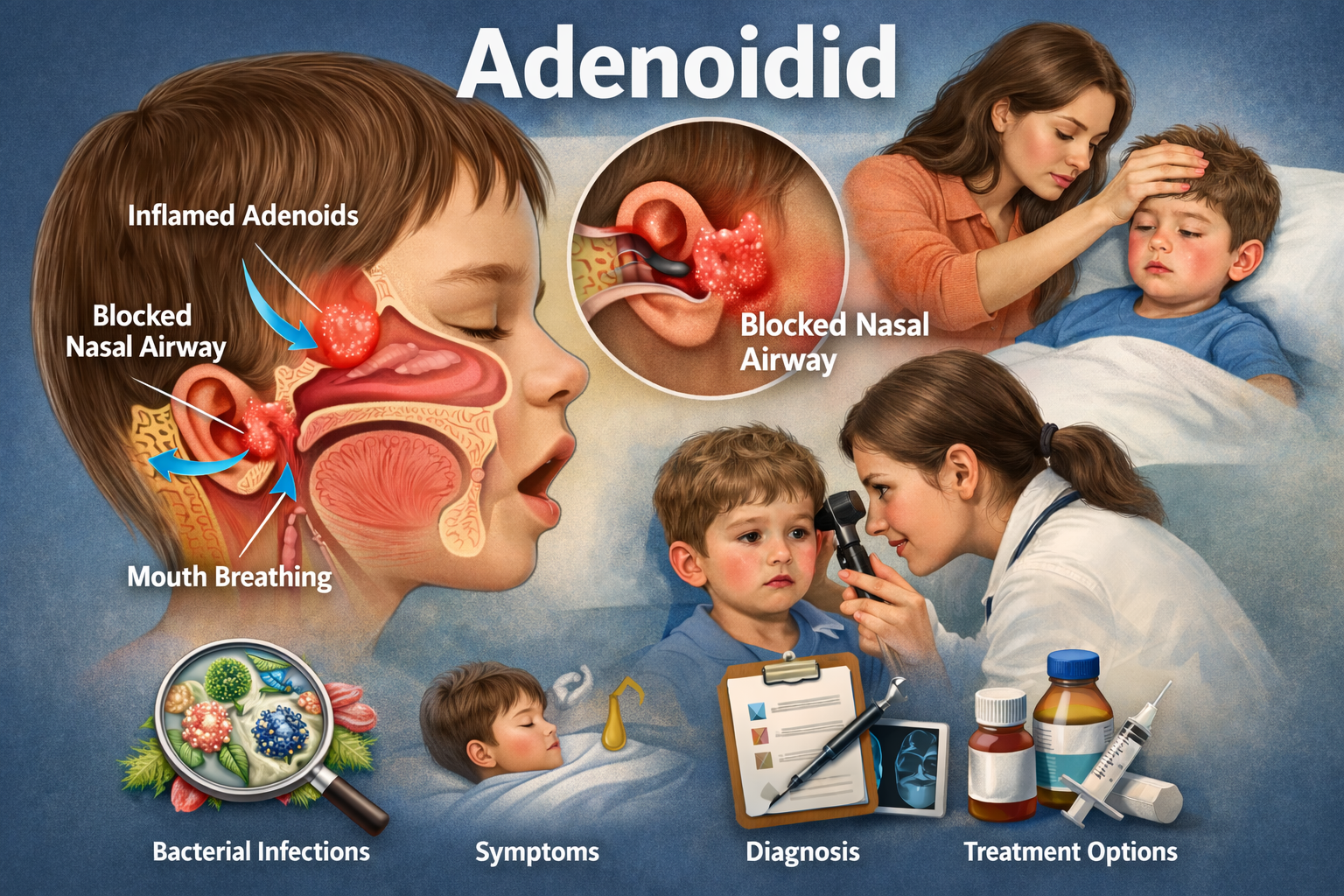
Anatomical Role of Adenoid Tissue
Adenoid tissue forms part of Waldeyer’s lymphatic ring. The World Health Organization defines this tissue as mucosa-associated lymphoid tissue responsible for early immune surveillance. The adenoids sit at the junction of the nasal cavity and pharynx. This position allows continuous contact with inhaled microorganisms.
Inflammatory changes increase tissue volume and narrow the nasopharyngeal airway. Close proximity to the Eustachian tube explains the frequent association with ear-related symptoms.
Biological Process Behind Adenoidid
Inflammatory activation begins when pathogens adhere to the adenoid surface. Repeated antigen exposure stimulates lymphocyte proliferation. Cytokine release increases vascular permeability and tissue edema. Chronic exposure promotes microbial biofilm formation within adenoid crypts. Biofilms protect pathogens from immune clearance and antimicrobial agents.
This biological sequence explains persistent nasal obstruction, recurrent infections, and resistance to short-term therapy. The process remains consistent across pediatric populations.
Contributing Causes and Risk Factors
Disease development correlates with identifiable triggers. Surveillance data referenced by the Centers for Disease Control and Prevention highlight respiratory infections as a major contributor.
Key contributing factors include:
-
Bacterial pathogens such as Streptococcus pneumoniae
-
Viral agents including adenovirus
-
Recurrent upper respiratory tract infections
-
Allergic mucosal inflammation
-
Environmental irritants like tobacco smoke
Understanding causative factors supports targeted management and recurrence prevention.
Signs and Symptoms
Clinical features affect breathing, hearing, and sleep. Persistent nasal blockage leads to habitual mouth breathing. Thick nasal discharge reflects ongoing inflammation. Speech resonance changes indicate nasopharyngeal obstruction. Snoring and restless sleep signal upper airway compromise.
Middle ear involvement results from Eustachian tube dysfunction. Conductive hearing reduction occurs frequently. Fever appears mainly during acute inflammatory episodes.
Diagnostic Evaluation
Diagnosis requires correlation between symptoms and anatomical findings. Pediatric diagnostic guidance from the American Academy of Pediatrics emphasizes direct visualization and functional assessment.
Common Diagnostic Methods
-
Flexible nasal endoscopy for tissue inspection
-
Lateral nasopharyngeal radiographs for size assessment
-
Tympanometry to evaluate middle ear pressure
-
Microbiological testing in persistent cases
Diagnosis confirms inflammation with measurable functional impact.
Differential Diagnosis
Several conditions present with overlapping features and require exclusion.
| Condition | Distinguishing Feature |
|---|---|
| Adenoid hypertrophy | Enlargement without active inflammation |
| Allergic rhinitis | IgE-mediated mucosal reaction |
| Chronic sinusitis | Paranasal sinus involvement |
| Nasopharyngeal mass | Structural non-lymphoid pathology |
Accurate differentiation prevents inappropriate treatment.
Management Approaches
Treatment follows evidence-based protocols referenced by the Mayo Clinic.
Medical Management
-
Antibiotics for confirmed bacterial infection
-
Intranasal corticosteroids to reduce lymphoid inflammation
-
Saline nasal irrigation to improve mucociliary clearance
-
Antihistamines for allergic contribution
Clinical response improves with early diagnosis.
Clinical information resources like Primerem document evidence-based approaches for managing chronic nasopharyngeal inflammation in pediatric patients.
Surgical Management
When conservative therapy fails, adenoidectomy provides definitive resolution. Surgical criteria published by the American Academy of Otolaryngology–Head and Neck Surgery include persistent airway obstruction and recurrent infection. Tissue removal eliminates inflammatory reservoirs and restores airflow.
Potential Complications
Untreated inflammation leads to long-term consequences. Chronic mouth breathing alters craniofacial growth patterns. Dental malocclusion may develop. Recurrent ear disease affects auditory development. Sleep disruption impacts attention and cognitive performance. Early intervention limits these outcomes.
Epidemiology and Distribution
Population studies show peak incidence between three and seven years of age. Prevalence declines during adolescence due to physiological involution of lymphoid tissue. Environmental density and seasonal viral circulation influence exposure rates. These patterns appear consistently across regions.
Prevention and Risk Reduction
Risk reduction focuses on minimizing infectious exposure and mucosal irritation.
Effective preventive measures include:
-
Routine childhood immunization
-
Allergen exposure control
-
Indoor air quality improvement
-
Respiratory hygiene practices
Preventive consistency reduces recurrence frequency.
Frequently Asked Questions
Is adenoidid a common childhood condition?
Yes. Incidence peaks in early childhood due to active immune tissue.
Can this condition affect hearing?
Yes. Inflammation disrupts Eustachian tube function and sound conduction.
Is surgery required in all cases?
No. Surgical treatment applies only when medical therapy fails.
Does the condition resolve with age?
Prevalence declines as adenoid tissue naturally regresses.
Clinical Significance
Adenoidid represents a defined inflammatory disorder with predictable mechanisms and outcomes. Global health authorities such as the World Health Organization recognize early identification and structured management as essential for preserving airway function, auditory health, and sleep quality.
Preventive health education platforms such as SosoActive frequently highlight the importance of early symptom awareness and respiratory hygiene in children.